Introduction:
Pyogenic granuloma (PG) or granuloma pyogenicum is a common tumor-like mucocutaneous overgrowth that occurs in the oral cavity or on the skin. It is considered to be non-neoplastic in nature, but a kind of inflammatory hyperplasia. The term pyogenic is used erroneously since this condition does not produce any pus.[1] Pyogenic granuloma is also known as pregnancy granuloma or pregnancy tumor when occurring in pregnant women, or as vascular eupulis, benign vascular tumor and haemangiomatous granuloma.[2]
"Hullihen S. P" in 1844 reported the first case of pyogenic granuloma which is probably the first case in the English literature[3]. It was again described in 1897 by two French surgeons, Poncet and Dor, who named this lesion otyomycosis hominis.[4] "Hartzell M. B in 1904 introduced the term "Pyogenic granuloma" or "Granuloma pyogenicum"[5]
Zafarzadeh et al (2006) defined pyogenic granuloma as an inflammatory overgrowth of the oral mucosa caused by minor trauma or irritation.[6] According to Neville et al (1998)[7], these injuries might be caused in the mouth by gingival inflammation due to poor oral hygiene, trauma or local infection, representing an exuberant tissue response. Gingival irritation and inflammation that results from poor oral hygiene, dental plaque and calculus or overhanging restorations may be precipitation factors in many cases[8]. The growth is typically seen in young adults; however it may occur in any age, especially in individuals with poor oral hygiene. Females are far more susceptible than males because of the hormonal changes that occur in women during puberty, pregnancy, and menopause.[9], [10] A preferences for children's has been reported by some investigators.[6]
Pyogenic granuloma of the oral cavity is known to involve gingiva commonly (75% of all cases),[12] uncommonly it can occur on the lips, tongue, buccal mucosa, palate and so on.[7],[12] Microscopically pyogenic granuloma is characterized by marked vascular proliferation amidst granulation tissue and chronic inflammatory infiltrate. When ulcerated, the surface of the lesion is covered with fibrin. Older lesions may present as fibrosis.[13] In view of its clinical characteristics, similar to some commonly occurring lesions in the oral cavity, the differential diagnosis of pyogenic granuloma includes Peripheral giant cell granuloma, Peripheral ossifying fibroma, Metastasis of malignant tumors, Haemangioma, Conventional granulation tissue, Inflammatory gingival hyperplasia, Kaposi sarcoma, Angiosarcoma and Non Hodgkins lymphoma.[7] Final diagnosis of the lesion is mainly by biopsy and histopathological examination.[7] Treatment of Pyogenic granuloma consists of surgical excision along with elimination of irritating local factors. We report an unusual case of pyogenic granuloma occurring in healthy pediatric patient.
Case Report
A 9 year old male patient was referred from department of pedodontics to the department of periodontics, Al Badar dental college and hospital for gingival swelling. The chief complaint of patient was discomfort in eating and unable to close the mouth completely. The lesion was of negligible size when the patient first noticed it (20 days back), but had grown over the past 20 days to attain the present size. No pain was associated with the lesion.
Extra oral examination did not reveal any facial asymmetry but lips were incompetent because of the extensive swelling. No abnormality was detected in temporomandibular joint and lymph nodes were not palpable. Intraoral clinical examination revealed solitary exophytic, sessile lesion, red in color, soft in consistency, with lobulations and bled easily on touch, extending from mandibular right central incisor to left canine involving both facial and lingual surfaces and from mucogingival junction to incisal plane (Fig - 1, 2). The size of the lesion was not in commensurate with the amount of local irritating factors present. There was grade I mobility in relation to 31 and 41. Intraoral periapical radiograph of that region showed minimal horizontal bone loss. Based on the overall clinical findings it was provisionally diagnosed as pyogenic granuloma or peripheral giant cell granuloma. The hemogram of the patient was within normal limits. Supragingival scaling was done and oral hygiene instructions were given. Excisional biopsy was done under local anesthesia. The biopsy specimen was sent for the histopathological examination. After complete hemostasis, periodontal pack was given and patient was recalled after one week. On recall visit periodontal pack was removed and satisfactory post operative healing was observed (Fig 3, 4).
Histopathological findings in the photomicrograph (Fig 5) shows stratified squmaous epithelium with pseudoepitheliomatous hyperplastic connective tissue with proliferating endothelial cells and fibroplasts. Neovascularization is prominent (Fig 6). Intense inflammatory infiltrate is seen comprising of lymphocytes, plasma cells and neutrophils, extravasated RBC's and necrotic tissue is also seen. The above histopathological findings are suggestive of pyogenic granuloma and final diagnosis of pyogenic granuloma was made.
Discussion:
Hyper plastic reactive lesions represent as a group the most common oral lesions, excluding caries, periodontal and periapical inflammatory disease. This group includes inflammatory gingival hyperplasia, oral pyogenic granuloma, peripheral giant cell lesion and peripheral cemento-ossifying fibroma[14]. In an analysis of 244 cases of gingival lesions
 | Fig 1: Intraoral view showing facial extension of pyogenic granuloma.
 |
 | Fig 2: Occlusal view of pyogenic granuloma showing facial and ligual extensions.
 |
 | Fig 3: Postoperative intraoral facial view.
 |
 | Fig 4: Postoperative occlusal view.
 |
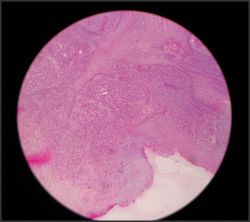 | Fig 5: Histological photomicrograph showing stratified squmaous epithelium with pseudoepitheliomatous hyperplastic connective tissue.
 |
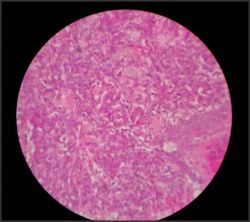 | Fig 6: Histological photomicrograph showing Neovascularization.
 |
in south Indian population, Shamim et al. found that these non neoplastic lesions accounted for 75.5% of cases with oral pyogenic granuloma being most frequent lesion, accounting for 52.71% cases[15].
There is consensus among many reviewers that pyogenic granuloma is reactional lesion formed in response to minor trauma or chronic irritation with reports of occurrences after low intensity traumatic injuries.[1],[2],[7],[11],[12], [13] Gingival irritation as a result of calculus, overhanging edges or rough restorations might be the predisposing factor for the development of gingival pyogenic granuloma. It is possible that micro ulceration from these irritants in an already inflamed gingiva allows the ingress into the gingival connective tissue of low virulent oral microflora. This evokes an exaggerated vascular hyperplastic response in the connective tissue resulting in the formation of pyogenic granuloma[16]. The other etiological factors considered are use of immunosuppressant drugs as reported by Bachymer et al[17] and Lee et al[18] in patients of graft versus host disease who were under cyclosporine. Development of Pyogenic granuloma as result of using Dried Freezed Demineralized Bone Graft and Extended Polytetraflouroethylene in regenerative periodontal surgical procedure was reported.[19] Kuo yuon et al have reported that imbalance between angiogenesis enhancers like Vascular endothelial growth factor, Basic fibroplast growth factor and angiogenesis inhibitors like Angiostatin may play a role.[20]
Although pyogenic granuloma may occur in all ages,[21] It is predominant in the second decade of life in young adult females, possibly because of the vascular effects of female hormones[9], [10] Studies done in Jordanian[1] and Singaporian[22] population is in agreement with this. Some authors believe that patients are mostly males less than 18 years of age, females in the age range 18 to 39, and older patients with an equal gender distribution.[23] In contrast to this, recent study by Epivationos et al reported that average age of the patient was 52 years with a peak incidence of occurrence in 6th decade of life and predominantly in women (1: 1.5).[24] With regard to site, gingival pyogenic granuloma is more common in the maxilla than in the mandible and in the anterior region than in the posterior regions of both jaws.[18],[25] Also, these lesions are more common on facial aspect than lingual, some extend between the teeth and involve both facial and lingual surfaces similar to the presented case. According to Villman et al[26] majority of pyogenic granuloma occur on marginal gingiva with only 15% accounting for alveolar part. In this case, lesion involved the alveolar part. Clinically, pyogenic granuloma is a smooth or lobulated exophytic lesion manifesting as small, red erythematous papule on a pedunculated or sometimes with sessile base, which is usually hemorrhagic and compressible. The size varies in diameter from a few millimeters to several centimeters[9], [10]. Rarely does PG exceed 2.5 cm in size and it usually reaches its full size within weeks or months, remaining indefinitely thereafter[27]. Clinical development of the lesion is slow, asymptomatic and painless, [9], [10] but it may also grow rapidly, [14] as reported in the present case. The surface is characteristically ulcerated and friable[28] which may be covered by a yellow, fibrinous membrane[17] and its color ranges from pink to red to purple, depending on the age of the lesion. Young pyogenic granulomas are highly vascular in appearance[9] because they are composed predominantly of hyperplastic granulation tissue in which capillaries are prominent. Thus minor trauma to the lesion may cause considerable bleeding, due to its pronounced vascularity[9], [17], whereas older lesions tend to become more collagenized and pink[9]. Rarely, PG may cause significant bone loss, as reported by Goodman-Topper and Bimstein[29]. In the presented case, there was a slight bone loss and the initial mobility of central incisors came back to normal after surgery.
Under histopathological examination pyogenic granuloma shows increased vascularity with increased endothelial cell proliferation resembling granulation tissue[30] and chronic inflammatory infiltrate dominated by plasma cells, lymphocytes and neutrophils[31]. Bhaskar SN, Jacoway JR[32] observed in their study that pyogenic granuloma is partly or completely covered by parakeratotic or non keratinized stratified squmaous epithelium. Major bulk of the lesion is formed by a non lobulated mass of angiomatous tissue. Usually lobulated lesions are composed of solid endothelial proliferation or proliferation of capillary sized blood vessels. Collagen in the connective tissue is sparse. The natural history of the lesion follows three distinct phases. In cellular phase, the lobules are compact and cellular with little lumen formation. In the capillary phase the lobules become highly vascular with abundant intraluminal red blood cells. In the involutionary phase there is tendency for intra and perilobular fibrosis with increased venular differentiation[27].
Pyogenic granuloma is a benign lesion; therefore, surgical excision is the treatment of choice although it may leave some visible scar. Although conservative surgical excision and removal of causative irritants (plaque, calculus, foreign materials, and source of trauma) are the usual treatments[9], [10], [33] for gingival lesions, the excision should extend down to the periosteum and the adjacent teeth should be thoroughly scaled to remove the source of continuing irritation[9]. Recently conservative surgical approaches to conventional surgery have been proposed, they include NdYag laser[34], Co2 laser[35], Flashlamp pulsed dye laser[36] and Cryosurgery[37]. These conservative treatments are usually adequate; however they can often result in visible scarring. Alternatively injections of absolute alcholol[38] and sodium tetradecyl sulphate sclerotherapy[39] are simple and effective in treating pyogenic granuloma without scarring but require multiple sessions. Series of intralesional injections of corticosteroids are effective for highly recurrent cases of pyogenic granuloma[40]. In the current case no recurrence was observed on follow up for 6 months.
Conclusion:
The current case was unusual in the sense it was occurring in a pediatric patient. There was rapid growth of the lesion involving both facial and lingual surfaces covering the entire central incisors and extending up to alveolar mucosa. There are few case reports in the literature with above findings. We were not able to elucidate history of trauma as patient was pediatric and parents were not able to recollect the history of trauma.
References:
1. Al-Khateeb T, Ababneh K. Oral pyogenic granuloma in Jordanians: a retrospective analysis of 108 cases. J Oral Maxillofac Surg. 2003; 61:1285-1288.
2. Graham RM. Pyogenic granuloma: an unusual presentation. Dent Update. 1996; 23:240-241.
3. Hullihen SP (1844). Case of aneurism by anastomosis of the superior maxilla. AM J Dent Sc 4, 160 - 162.
4. Sanjay Venugopal et al. Pyogenic granuloma a case report. J Dent Sc & Res 1; 1: 80 - 85.
5. Hartzell MB (1904) Granuloma pyogenicum. J Cutan Dis Syph 22, 520-525.
6. Hamid Jafarzadeh. Oral pyogenic granuloma: A review. J Oral science 2006 ;48(4):167-175.
7. Neville BW, Damm DD, Allen CM. Patologia e oral maxillofacial. Rio D Janiero. Guanabara, Koogan, 1998.
8. Angelopoulus AP. Pyogenic granuloma of oral cavity: Statistical analysis of its clinical features. J. Oral Surgery 1971; 29: 840-845.
9. Neville BW, Damm DD, Allen CM, Bouquot JE. Oral & maxillofacial pathology. 2nd ed, Philadelphia: WB Saunders; 2002. p. 437-495.
10. Regezi JA, Sciubba JJ, Jordan RCK. Oral pathology: clinical pathologic considerations. 4th ed, Philadelphia: WB Saunders; 2003. p. 115-116.
11. Lin RL, Janniger CK. Pyogenic granuloma. Cutis. 2004;74:229 - 233.
12. Damm DD, Fantasia JE. Elevated and ulcerated nodule of lip. Pyogenic granuloma. Gen Dent. 2002;50:466-468.
13. Regezi JA, Sciuba JJ. Oral pathology, clinical pathological correlations. Philadelphia: Saunders; 1989.
14. Esmeili T, Lozada-Nur F, Epstein J. Common benign oral soft tissue masses. Dent Clin North Am. 2005 ; 49: 223-240.
15. Shamim T, Varghese VI, Shameena PM, Sudha S. A retrospective analysis of gingival biopsied lesions in south Indian population:2001-2006. Med Oral Pathol Oral Cir Bucal.2008;13(7): 414-418.
16. Bragado R, Bello E, Requena L, Renedo G, Texeiro E, Alvarez MV, Castilla MA, Caramelo C. Increased expression of vascular endothelial growth factor in pyogenic granulomas. Acta Derm Venereol 1999;79: 422-5.
17. Bachymeyer C, Devergie A, Mansouris Set al. Pyogenic granuloma of the tongue in chronic graft vs host disease. Ann Dermatol venerol 1996; 123: 552 - 554(in french).
18. Lee L et al. Intraoral pyogenic granuloma after allogenic bone marrow transplant, report of three cases. Oral surg, Oral med, Oral pathol 1994; 78: 607 - 610.
19. Fowler FB et al. Pyogenic granuloma associated with GTR: A case report. J Periodontol 1996; 67: 1011 - 1015.
20. Kuo Yuon, Ying - Tai Jin, Ming T. lin The detection and comparison of angiogenesis - associated factors in Pyogenic granuloma by immunohistochemistry. J Periodontol 2000; 71: 701 - 709.
21. Lawoyin JO, Arotiba JT, Dosumic OO. Oral pyogenic granuloma: A review of 38 cases from Jhadan, Nigeria. Br J Oral Maxillofac Surg 1997; 35:185-189.
22. Zan RB, Khoo SP, Yeo JF (1995) Oral Pyogenic granuloma (excluding pregnancy tumor) - a clinical analysis of 304 cases. Singapore Dent J 20, 8 - 10.
23. Pilch BZ. Head and neck surgical pathology. Lippincot Williams & Wilkins, Philadelphia 2001; 389 - 390.
24. Epivatianos et al. Pyogenic granuloma of the oral cavity: Comparitive study of its clinicopathological and immunohistochemical features. Pathol int 55, 2005 : 391 - 397.
25. Bragado R, Bello E, Requena L, Renedo G, Texeiro E, Alvarez MV, Castilla MA, Caramelo C. Increased expression of vascular endothelial growth factor in pyogenic granulomas. Acta Derm Venereol 1999;79: 422- 425.
26. Vilmann A, Vilmann P, Vilmann H. pyogenic granuloma: evaluation of oral conditions. Br J Oral Maxillofac Surgery 1986; 24: 376 - 382.
27. Sternberg SS, Antonioli DA, Carter D, Mills SE Oberman H. Diagnostic surgical pathology 3rd Ed Philadelphia: Lippincott Williams & Wilkins; 1999.p. 69, 174.
28. Greenberg MS, Glick M. Burkett's oral medicine: diagnosis and treatment. 10th ed, Hamilton: BC Decker; 2003. p. 141-142.
29. Goodman-Topper ED, Bimstein E. Pyogenic granuloma as a cause of bone loss in a twelve-yearold child: report of case. ASDC J Dent Child 1994;61:65-67.
30. Kerr DA. Granuloma pyogenicum. Oral surg Oral med Oral Pathol 1951; 4:158-176.
31. Eduardo Sanches Et al. Pyogenic granuloma on the upper lip: An unusual location. J App Oral Sci 2010; 18(5) 538 - 541.
32. Bhaskar SN, Jecoway JR. Pyogenic granuloma clinical features, incidence, histology and result of treatment. Report of 242 cases. J Oral surgery 1966; 24: 391-398.
33. Eversole LR. Clinical outline of oral pathology: diagnosis and treatment. 3rd ed, Hamilton: BC Decker; 2002 p. 113-114.
34. Powell JL, Bailey CL, Coopland AT et al. Nd Yag laser excision of a giant gingival pyogenic granuloma of pregnancy. Lasers surg Med 1994; 14 : 178 - 183.
35. White JM, Chaudhary SI, Kudler et al. Nd Yag and Co2 laser therapy of oral mucosal lesions. J Clin Laser Med Surg 1998; 16: 299 - 304.
36. Meffert JJ, Cagna DR, Meffert RM. Treatment Of oral granulation tissue with Flashlamp pulsed dye laser. Dermatol Surg 1998; 845 - 848.
37. Ishida CE & Ramos C Silva. Cryosurgery in oral lesions. Int J Dermatol 1998; 37: 283 - 285.
38. Ichimiya M, Yoshikawa Y, Hamamoto Y et al. Successful treatment of pyogenic granuloma with injection of absolute ethanol. J dermatol 2004; 31: 342 - 344.
39. Moon SE, Hwang EJ, Cho KH. Treatment of pyogenic granuloma by sodium tetradecyl sulphate sclerotherapy. Arch dermatol 2005; 141: 644 - 646.
40. Parisi E, Glick PH, Glick M. Recurrent intraoral pyogenic granuloma with corticosteroids. Oral Dis 2006; 12: 70 - 72. |